How insurers use secret definitions to avoid paying ill customers
By Elizabeth McArthur
When Mary* was diagnosed with multiple sclerosis (MS) she found herself facing a lot of uncertainties. Not least of all, Mary wondered how she would make ends meet long-term.
At the time, she was working for the Commonwealth Bank and commuting into the city every day.
Mary kept her job for as long as she could; she still describes herself as a hard worker and someone who takes pride in what she does.
But, as her illness progressed it became clear Mary wasn't going to be able to stay in full time work until she was retirement age as most of us imagine we will.
That's when the worries about finances really started. Working out how to pay for simple living expenses suddenly seemed to involve impossible sums.
Mary was attending a support group for people with MS when she heard about a business that helped other people in the group access Centrelink and make insurance claims.
That business was ClaimRight, a company set up by financial adviser William Johns which helps people apply for Centrelink payments and for insurance they might be eligible for through their super funds. The business operates on a no-win, no-fee basis.
Mary had three super funds. One was from her time working at St George Bank, another was from a job she had with Telstra and the third was from her job at the Commonwealth Bank.
She didn't realise that she had been paying fees through each of these funds for insurance policies.
What might have been poor financial planning in most cases turned out to be a blessing in disguise though - Johns and his team explained to Mary she was entitled to claim total and permanent disability (TPD) through each of the super funds. Each claim was likely to result in a lump sum payment.
Two of Mary's super funds, the ones she had when she worked at Telstra and St George Bank, accepted that her MS diagnosis meant she wouldn't be able to work again and paid out her TPD claim.
However, Mary was told she'd need a lawyer to help her access the CommInsure TPD cover she held through her Commonwealth Bank staff super plan, because her MS didn't meet CommInsure's definition of MS.
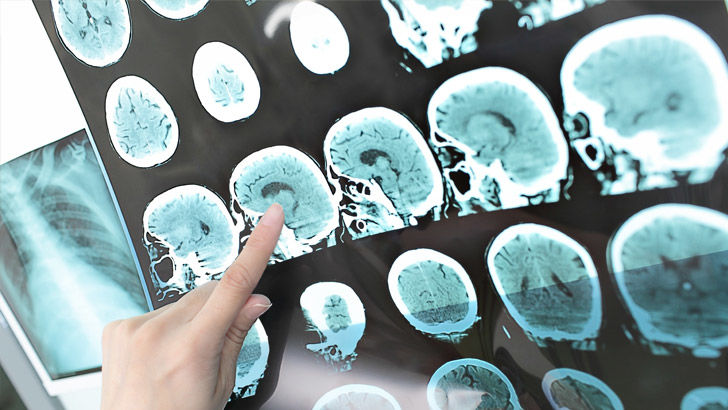
The definition CommInsure was upholding states that MS must be characterised by "demyelination in the brain and spinal cord".
Demyelination refers to the lesions (also sometimes known as white matter or scar tissue) that occur in the central nervous system of MS sufferers. It's these lesions that cause the symptoms of MS, making it hard for the brain to send signals to the rest of the body.
Mary only has lesions in her brain. They affect her vision and balance and cause fatigue and concentration issues.
"My neurologist was quite upset to hear what CommInsure is claiming is the definition," she says.
"My specialist spoke to CommInsure, wrote to them, sent them documents and tried to tell them the definition of MS and how it is diagnosed. You don't necessarily need lesions on the brain and the spine."
Shine Lawyers solicitor Katryn Strong is representing Mary. She describes someone with MS finding out that they don't meet an insurer's definition of the illness as a "ridiculous" situation.
"If someone has diagnosed MS they have MS, there is no grey area with this awful disease. Mary should be paid her total and permanent disability payment, no questions asked," Strong says.
"Mary has intensifying symptoms, her deterioration is challenging enough to cope with. The last thing she needs is an insurer denying her a payment she rightly deserves."
Mary says she doesn't understand why so many other organisations acknowledge her illness, but CommInsure holds her up to a different standard.
"I have NDIS help, I'm on a disability pension but CommInsure are arguing whether I have MS? They want to see lesions in the spine and the brain? It doesn't make sense. I guess that's what insurers do, they keep their money for as long as they can," Mary says.
"People with MS have to suffer to get what they should get in the first place. They get put through the mill. They have anxiety and depression and are trying to work out where the next income is coming from."
CommInsure responded to enquiries about the definition of MS applied to Mary by pointing out that in August 2020 CommInsure updated its definition of MS for retail policies (life insurance policies sold through a financial adviser, not those available in super funds).
The new definition removes any reference to demyelination or where it should be found. CommInsure says it is currently in the process of offering this updated definition to insurance in super. However, that doesn't change the situation for Mary and others like her.
"In employer policies in superannuation, TPD claims are typically assessed on whether the member has been absent from work for a period of time and is unlikely to be able to work ever again. Some policies also include a 'Day 1' TPD definition for defined medical conditions, which pays out on diagnosis without requiring an absence from work," a spokesperson for CommInsure clarified.
"The policy in question contains a Day 1 TPD definition which covers multiple sclerosis (MS). If a member does not meet the definition for their condition to trigger a 'Day 1' payment, they will still be assessed against the standard TPD definition that looks at their capacity to work ever again."
'Day 1' TPD simply means that clause in the policy about being absent from work for a certain period of time doesn't apply because a diagnosis or injury is so severe it results in someone being unlikely to work ever again.

CommInsure has been caught out over its medical definitions before. A case study in the Royal Commission looked at CommInsure's definition of a heart attack, which required a certain amount of the chemical troponin to be present in the body.
It was a medically inappropriate definition, one doctors disagreed with and one that saw people who had genuinely suffered heart attacks denied payments on insurance policies they had paid fees for.
Also mentioned during the Royal Commission was CommInsure's definition of breast cancer which required cancer patients to have "radical breast surgery" to be eligible to claim. However, what constituted "radical breast surgery" was not clearly defined and the definition was found by the Royal Commission to be severely outdated.
CommInsure isn't the only insurer to use a definition of MS that MS patients, neurologists, lawyers and MS Australia disagree with.
Integrity Life, NobleOak, Zurich, MLC Life and ClearView all use definitions of MS that refer to lesions, demyelination or white matter as needing to be identified on the brain and spinal cord.
TAL and NEOS Life refer to demyelination as needing to be identified in the brain and/or spinal cord. OnePath's definition says neurological investigations should find evidence of lesions in the central nervous system. Mary would have met these definitions.
Reviewing a list of the MS definitions used by 14 life insurers in Australia, MS Australia national policy officer Andrew Giles found the vast majority to be "too specific" and not in line with current medical thinking.
AIA got a positive mention from Giles, as its definition only requires MS to be diagnosed by a neurologist. BT's definition is similar, requiring diagnosis by an appropriate medical professional and a history of at least one episode.
A definition from NobleOak (from a PDS branded Australian Unity) was particularly problematic to Giles. It requires MS to be diagnosed by two neurologists and for white matter to be identified in the optic nerves, brain stem and spinal cord.
Requiring an MS patient to see a second neurologist is nonsensical, says Giles, pointing out that patients often face long waiting lists just to see one neurologist and appointments with neurologists are expensive.
"Post-diagnosis people are lucky to get 10 minutes a year with a neurologist and it's expensive," says Giles.
"Why do you need to go to two? One neurologist can look at an MRI and if they're happy to write a report confirming a diagnosis of MS, why would you have to go to a second neurologist?"
Many of the insurers also refer to specific testing they expect to see as evidence of MS - lumbar punctures and MRIs in particular.
What insurers might not think of, says Giles, is the physical and psychological toll these tests take on MS patients. He's concerned some people might be sent for a second or third round of testing that is not medically necessary in an attempt to meet the definitions used by insurance companies.
"A lumbar puncture is awful. It's a huge needle going into your spine and sucking out fluid. You have to have painkillers and go to hospital for it. It is awful," says Giles.
"An MRI is pretty awful for a lot of people too. You get on the little table and you're stuck in this tunnel - a lot of people need some Valium to get through it because it's like being pushed into a coffin. Then these huge magnets spin around the outside and make this huge noise at about 120 decibels. For some people, it takes counselling to have an MRI."
Maurice Blackburn lawyer Josh Mennen says, unfortunately, he isn't too surprised to hear Mary's story - especially after the Royal Commission case studies.
And, he says, it's not going to be straight forward for consumers to educate themselves. Especially when insurance is only held through super, finding a full list of the definitions used by an insurer is not an easy task - let alone reading it.
"For a consumer, reading these documents is just going to be a labyrinth of confusion," says Mennen.
"There's no benchmark industry standard to these definitions based on proper medical consultation. I think part of the problem is that some insurance companies are not consulting with the appropriate medical specialists."
Mennen points out that the Life Insurance Code of Practice requires medical definitions to be reviewed regularly and in keeping with contemporary science.
"I would suggest that the insurers using these definitions are not complying with that obligation," says Mennen.
"I think this is something the corporate regulator, ASIC, should be looking into because it now has product intervention powers that would enable it to compel the insurer to provide a reasonable product to consumers if the insurer is refusing to do so itself.
"From an individual legal perspective for consumers, I think there is a strong argument to be made that insurers who are offering these inappropriately harsh medical definitions are in breach of their legal obligations to act in the utmost good faith by knowingly providing an obsolete product."
Unfortunately, Mennen suspects very specific medical definitions might play a sinister role in the business models of some insurance companies.
"If insurers have to pay a client then, generally speaking, they try and write the cheque slowly because as long as the money sits with the insurer they are able to invest it and that's how they make money. So, if it's the case that these definitions cause delays - does that benefit the insurer?"
*Mary prefers not to have her last name published for privacy reasons.
Get stories like this in our newsletters.



